5 space robots that could heal human bodies—or even grow new ones

IN ONE OF HUMANITY’S many possible futures, the fearless explorers tasked with climbing cloud-splitting mountains in oxygen-poor atmospheres or charting the low, darkened craters of various alien landscapes would never perish from injuries during perilous scouting expeditions. Nor would they fall ill or sustain genetic damage, thanks to supercharged hypersleep chambers that would heal otherwise fatal wounds. As it is today, astronauts don’t have the luxury of being unprepared—instead they must be equipped to deal with all sorts of medical mishaps, especially as they experiment with long-term spaceflight beyond the far side of the moon.
Current human-rated spacecraft come stocked with emergency supplies to assist the crew, mostly everyday things like Band-Aids and aspirin, but also more specialized items like hydromorphone injections and those all-too-famous space blankets. While astronauts on the International Space Station (ISS) have relied on these, as well as telemedicine calls, to treat ailments and keep a clean bill of health, the fact is, being on another world could put a serious dent in the capacity of emergency medical care. NASA notes that all crew members are trained to handle the medical devices on board—but if a complex surgery is needed and the patient can’t be quickly flown back to Earth, the trainees would have to forge on with limited tools and experience. Thankfully, the worst they’ve faced so far is blood clots.
To plan for these inevitable crises, space agencies have latched on to the science of 3D bioprinting to help revolutionize regenerative medicine for life in the cosmic abyss and on the ground. Researchers have already made strides in bioprinting—the process of generating living cells and medical products in a manner similar to 3D printing—creating tissues, skin grafts, and eventually, whole organs for future transplants, as well as artificial bones that could become “spare parts” for injured astronauts.
But as demand for smaller, more compact technologies grows, another class of machines has been rocketing to new heights. Capable of stretching, squeezing, bending, and even twisting to fulfill their tasks, “soft robots” are fabricated with materials inspired by living tissue such as human skin, instead of the rigid structures used in traditional remote-controlled systems. This allows robotic instruments to interact more safely with our bodies and lets surgeons perform complicated procedures with more accuracy and precision, says Sheila Russo, an assistant professor at Boston University who specializes in mechanical engineering design for miniaturized surgical robots.
“I work in a field where we build robots that can help patients survive,” Russo explains. “We as engineers listen to people that have problems, and we want to engineer a robotic solution to it.” She likes to point to Big Hero 6’s Baymax as a fictional example of an autonomous soft robot that successfully heals people, either with the various medical devices it’s equipped with or by offering helpful advice.
Though the doodads in development won’t be able to simply hug anyone’s aches and pains away (yet), they’re lightweight and relatively cheap to produce, making them easy to transport to remote locations, says Russo. For instance, one lab at King’s College in the UK is trying to address the limitations of ultrasound by creating adaptable soft robots that can withstand high-energy sound waves.
As these prototypes gain traction within the greater medical field, there’s still a long list of quirks and challenges to tackle. But their endless potential could help humans endure extreme circumstances both on Earth and in the stars.
Flexible In Situ 3D Bioprinter
Dream Team: The University of New South Wales
Function: Swiss Army knife
ETA: 5–7 years

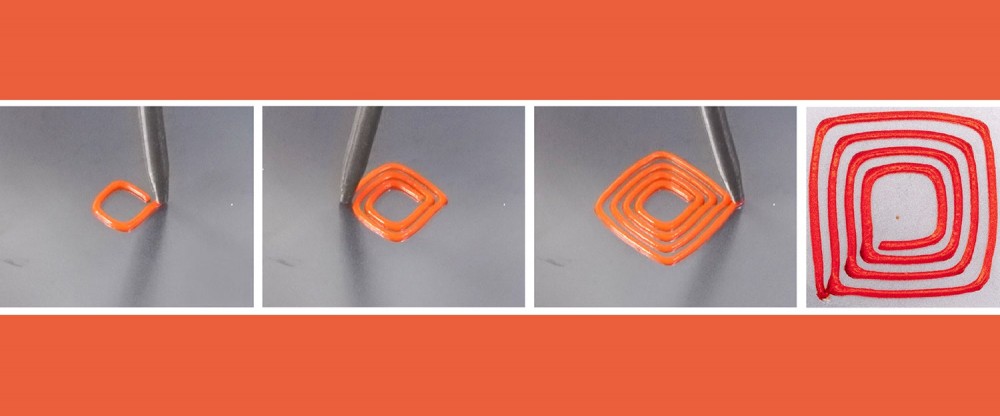
Acting much like a medical endoscope, this tiny, multifunctional robotic arm (about 0.8 inches in diameter) can be used to fix damaged body parts directly inside a patient’s body. Conventional devices rely on large desktop printers to create artificial tissues, which can then either be kept and grown until mature or implanted directly into the body. But this high-cost method often poses risks, such as structural damage to the faux organ during transport, tissue injuries, and contamination once the part is brought out of a sterile environment.
The flexible in situ 3D bioprinter (F3DB), on the other hand, works by accessing hard-to-reach areas of the body via small incisions or through natural orifices such as the mouth or anus. “About 90 percent of the human body has a tubular structure,” says Thanh Nho Do, a senior lecturer at UNSW Sydney and one of the team leads for the project. “If you can develop the technology, [robots] can navigate along this way in any desired direction.”
Once positioned in the target area, F3DB’s multiaxis printing head, which is mounted on a snakelike extendable arm, bends its nozzle to print in three different directions, delivers water to wash away blood and tissue, and acts as an electric scalpel to flag and sever cancerous lesions or tumors. It’s so versatile in its applications that it could potentially be used as an all-in-one surgical tool for medical professionals, says Do.
Although this tool is still more than half a decade away from human trials, researchers plan to continue using haptic technology—sensor-filled gadgets that can convey tactile information—to manipulate the device, so the system could one day be easily controlled in extreme environments, such as on space stations or in lunar or Martian settlements.
The 3D BioFabrication Facility
Dream Team: Redwire Space
Function: Knee replacement
ETA: 5–10 years

A recent addition to the ISS, the 3D BioFabrication Facility (BFF) and Advanced Space Experiment Processor are two separate payloads that combine to make a powerful 3D bioprinting laboratory. In collaboration with the ISS National Lab and the Uniformed Services University of the Health Sciences Center for Biotechnology, Redwire’s researchers plan to use it to re-create part of a human knee in space—specifically the meniscus, cartilage that helps absorb shock and stabilizes the joint. If successful, it could be the first step in helping to treat severe knee injuries for US military service members on Earth.
“A torn meniscus is one of, if not the most common issue that our military have,” says Ken Savin, the aerospace manufacturing company’s chief scientist. “[It’s] a day-to-day issue that a lot of people have and translates to the general population, so it’s a great target to go after.” The printer itself, which is about the size of a dorm fridge, cultures pre-harvested adult stem cells into a solution called bio-ink.
After being warmed, fed with liquid nutrients, and stimulated to grow, the mixture can be layered into precise, ultrafine structures aboard the ISS and then shipped back to Earth. Strong gravitational forces cause the soft tissues to spread apart like puddles of water, but in space, they can be expected to hold their form due to the microgravity inherent to the ISS, says Savin.
“When you remove gravity, you open up a whole new field of science,” Savin says. “It allows you to do things and see things that were otherwise hidden.” Once the ISS is decommissioned (which will happen after 2030), Redwire aims to continue advancing its biomanufacturing research aboard Blue Origin’s planned space station, Orbital Reef.
While the company is now still in the early planning stages of the meniscus project, Savin expects it to be a stepping stone to many other medical breakthroughs, including individualized heart patches that restore cardiac function. Depending on the size of the 3D-printed tissue, production would likely take less than a day. And that’s not the only way BFF would move anatomical technologies along. With future commercialization, the portable lab could help organ-donation hopefuls avoid long wait times and subpar inorganic replacements.
The Soft Growing Robot
Dream Team: University of Minnesota
Function: Infinitely stretching tube
ETA: 10+ years

Inspired by plant roots, pollen tubes, and fungi, engineers at the University of Minnesota recently developed a process that allows soft robots to exhibit a level of movement called tip growth, previously seen only in nature. Organisms use this method to add new cells to the ends of their bodies, enabling them to generate large, specific structures over time, cross harsh terrain with ease, and navigate via external stimuli like light or chemical signals.
In 2022, researchers were able to mimic this process in their own robotic prototype by using a technique called photopolymerization, which uses light to transform liquid molecules into solid materials. It’s a popular 3D-printing strategy in the medical field, specifically for creating accurate anatomical models of patients’ bodies, but in this novel application, it allows a soft robot to build its own body from a liquid monomer solution as it navigates complex environments.
Capable of a number of exploratory tasks as it slinks along its path, this inchworm-like device can grow up to speeds of about 5 inches per minute, stretch up to about 5 feet, and avoid and even deflect obstacles to reach the deepest recesses of the human body. The tool could be especially helpful for medical fields like gynecology and urology, according to Timothy Kowalewski, an associate professor of mechanical engineering at the University of Minnesota and a member of the project. He also sees it making a difference in procedures like automated intubation and heart attack treatment, where soft catheters are pushed through blood vessels to stabilize a patient.
The BioPrint FirstAid Handheld Bioprinter
Dream Team: The German Aerospace Center
Function: Cellular Band-Aid
ETA: 5–10 years

Not all soft robots are meant to turn humans into cyborgs with fancy mechanical parts. One bioprinter prototype, developed by the German Aerospace Center, was designed to accelerate an astronaut’s own healing process, says Michael Becker, the project manager for the program.
Like other innovations in space-centered healthcare, the BioPrint FirstAid Handheld Bioprinter will use cells collected from astronauts before the mission to prepare cartridges of personalized bio-ink for emergency wound treatment, like fixing up superficial lesions and even bone fractures. Likely the first-ever handheld version of a bioprinter in space, the device resembles a compact glue gun—complete with a printing head, guide wheels, and room to hold two bio-ink cartridges for easy access and use.
While the machine was created to be completely manually operated, the actual printing process takes only a few minutes, Becker explains. “You basically put the printer on your arm or somewhere else and drive over the injured skin.” The nozzle then pushes the solution out to create a plaster-like wound covering. In 2021, ESA astronaut Matthias Maurer demonstrated the technology using simulated cells during a training session on Earth, and he did it again in 2022 during his Cosmic Kiss mission on the ISS.
Having a handheld bioprinter along on a long-duration spaceflight would allow the crew to quickly provide personalized medical care, but the creators need to clear two hurdles first: determining just how many bio-ink cartridges would be needed for a given interplanetary journey and figuring out how to store them in a stable environment. “The challenge right now [is] to create ink where these cells can survive for long-term missions,” says Becker.
The team hopes the astronaut-friendly tool finds alternative uses, such as in research missions to harsh environments like Antarctica or for bedridden patients.
The Ferromagnetic Soft Catheter Robot
Dream Team: Huazhong University of Science and Technology
Function: Magnetic bioprinter
ETA: Decades
Another robot designed to print tissues and organs inside the human body in a minimally invasive manner, the ferromagnetic soft catheter robot (FSCR) stands out from its counterparts because it relies on magnets to move about.
“This work provides two very new ideas,” says Jianfeng Zang, a professor at Huazhong University of Science and Technology whose work revolves around bridging the gap between hard machines and the soft human body. “One, in that we can do minimally invasive bioprinting, and the second one is that we use a magnetic system to do it.”
Usually, these kinds of medical machines use motors to propel themselves through the patient’s body. But Zang’s group disperses particles of the rare-earth metal neodymium down the center of their catheter-shaped robot, which also doubles as a bioprinter capable of fabricating complex structures. The device can be swiftly steered via an external computer-controlled magnet to transport materials like drugs or injectable bio-inks through narrow, winding environments. It’s also highly durable because neodymium retains its magnetism for hundreds of years.
Researchers are working to miniaturize the device, which is currently a fraction of an inch, even further. It could one day offer physicians finer control over the instrument’s movements and allow them to complete complex procedures without radioactive X-rays.
“We just want to use magnetic robots to treat some disease or do some precise surgery that existing technology cannot do,” says Zang. “It’s our dream.”
Read more PopSci+ stories.